COVID-19 BEST PRACTICES
AIOT JOINT STATEMENT
27 April 2020
The outbreak of a novel coronavirus, referred to as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) or coronavirus disease-19 (COVID-19) has rapidly become a global public health threat, endangering the health and well-being of all people, but especially vulnerable populations. The pandemic has also precipitated social disruption, exceptional health-care utilization, and economic instability worldwide. Limiting further spread of COVID-19 has become the singular focus, with unprecedented international collaboration and rapid dissemination of emerging scientific evidence. The Alliance of International Organizations of Orthopaedics and Traumatology (AIOT) agreed on a number of over-arching best practices to guide our international members. AIOT recommends global research collaborations to maximize efficiency and existing networks during COVID-19 to determine impacts of the pandemic on orthopaedic and trauma care worldwide.
This statement does not replace those of member organizations, rather it provides a unification of key recommendations.
KEY RECOMMENDATIONS
General considerations
- Ensure patient and staff safety.
- Keep up-to-date regarding evolving clinical guidelines, as well as your institution capacity issues relative to the regional pandemic severity.
- Judicious use of Personal Protective Equipment (PPE) and prepare contingency plans for supply shortages.
- Establish rotating teams that can work in isolation of each other.
- Postpone elective surgeries. Only schedule urgent or emergent surgical cases.
- Develop a plan for phased return of elective and non urgent procedures.
- Promote tele-health modalities to increase access for diagnostic and rehabilitation purposes.
- Use technology to help trainees engage in remote knowledge and skill acquisition
training. - Senior Consultants should be available to actively support trainees.
Outpatient care and elective procedures
- Screen patients and personnel attending outpatient and in-patient facilities for COVID-19.
- When possible, help reduce emergency departments workload by extending operating hours of outpatient clinics and increase their resolution capacity.
- Schedule clinics in line with social/physical distancing principles.
- Prior to determining definitive management of semi urgent or other controversial cases seek for senior surgeons’ advise.
- Minimize imaging requirements. Avoid images that are unlikely to change patients’
management. - Prevent unnecessary follow-up appointments.
- The local epidemiological situation and availability of resources should be considered before planning to resume elective surgeries. Develop protocols and be cautious. Stay prepared for a rapid scale-down in case pandemic severity worsens.
Urgent/emergent procedures and risk mitigation strategies
- Implement a surgical review committee to assist in surgical cases prioritization. Develop clear policies for airway management in known/suspected COVID-19 patients.
- Develop a dedicated COVID-19 operating room:
1) Away from high traffic areas;
2) Physical or taped-off anteroom;
3) Negative pressure where available (or turn off positive pressure and air conditioning).
- Develop independent flow pathways for traffic in and out of designated COVID-19 OR.
- If possible, plan surgeries as day-cases aiming for an early discharge and single- staged surgeries.
- Perform interventions only if documented treatment effects are superior to non- operative management. Discuss benefits and harms with patients.
Consolidation of 83 published recommendations.
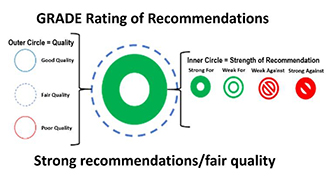 The strength and quality of each recommendation was assessed using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach. This determines the quality of evidence to be either good, fair or poor; and the strength of evidence to range from strong recommendation for, to strong recommendation against.
The strength and quality of each recommendation was assessed using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) approach. This determines the quality of evidence to be either good, fair or poor; and the strength of evidence to range from strong recommendation for, to strong recommendation against.
Contributors (in alphabetical order):
Jamal Ashraf (Secretary General, APOA), Onder Aydingoz (Past President, EFORT), Mohit Bhandari (Research Academy Chairman, SICOT), Horacio Caviglia (President, SLAOT), Ali Hassan Chamseddine (Past Vice President, PAOA), David Choon (Immediate Past President, APOA), Mohamed Darwish (President, PAOA), Mahmut Nedim Doral (President, APOA), John Dormans (President, SICOT), Francisco Forriol (Vice President, SLAOT), Klaus-Peter Günther (First Vice President, EFORT), Philippe Hernigou (Treasurer, SICOT), Vikas Khanduja (Education Academy Chairman, SICOT), David Limb (Secretary General, EFORT), Edward T Mah (Past President, APOA), Philippe Neyret (President, EFORT), Shanmuganathan Rajasekaran (Immediate Past President, SICOT) and James Waddell (Secretary General, SICOT).
- Download Full statement | PDF Document | 3 pages | 500kb
Other AIOT Statements:
- 12 June 2020 | AIOT Joint Statemet on Human Rights | PDF Version
AIOT is the joint platform of five leading international organizations of orthopaedics and traumatology. It was established to increase collaboration and facilitate communication among member organizations in 2018.
AIOT member organizations (in alphabetical order):
- APOA (Asia Pacific Orthopaedic Association)
- EFORT (European Federation of National Associations of Orthopaedics ad Traumatology)
- PAOA (Pan Arab Orthopaedic Association)
- SICOT (Société Internationale de Chirurgie Orthopédique et de Traumatologie)
- SLAOT (Sociedad Latinoamericana de Ortopedia y Traumatología)
KEY RESOURCE
Best Practices for Surgeons: COVID-19 Evidence-Based Scoping Review, A Unifying Report of Global Recommendations, Version 2.0, Published April 23, 2020. Prada C, Chang Y, Poolman R, Johal H, Bhandari M. Access full report click: https://myorthoevidence.com/covid19